After the last article on this theme I got many questions, and decided to write a follow up article in TCCC starting with MARCH and moving on from there. TCCC is a creation of U.S. Special Operations Command and medical personnel to create the optimal combat medicine to save more lives. With TCCC it is estimated a decrease of combat death from 24% to 3%. The goal is to reach hospital alive.
Let us start with MARCH, an initialism mnemonics for the essence of TCCC the initial steps. MARCH indicate M – Massive haemorrhage, A – Airway, R – Respiration, C – Circulation and H – Head/ Hypothermia. This is a first aid system specialized in situations related to conflict. Let me guide you step by step through this system before I discuss related aspects and themes to TCCC. MARCH in TCCC only makes sense when we see it in the correct context; the three areas of first aid: Care under Fire (CUF), Tactical Field Care (TFC) and Tactical Evacuation Care (TACEVAC). In a tactical operation you will be under pressure, it might be dangerous and you might be seriously hurt. TCCC is developed for helping us to survive in these situations and to help in the best way possible.

Let me walk you through the system: A hot situation occurs and you are in it. One of you team is injured and you as the tactical paramedic need to help him through the MARCHE protocol.
Care under Fire
The first point is: Care under Fire (CUF). It is possible and likely that somebody might shoot at you. That is why you need to consider “SSS” – Security, Scene and Situation. SSS mean first you take care of your security and not put you in more risk than needed. A tactical paramedic need to be more careful than a normal soldier. He is there to help wounded and not directly there for the intervention. The second step is Scene. This is an evaluation of the place, how it looks like, the dangers it present and how to use it favourable. This is Situation. Here you evaluate what is going on, the presence of danger and what you should do as a tactical paramedic. Normal paramedics should not enter hot zones, but tactical paramedics are trained for hot and dangerous scenes. If the tactical paramedic evaluates the security to be sufficiently safe he will go in.

The basic TCCC structure for CUF is divided into seven steps. First return fire and take cover. Move the injured to a safer place. If possible, quickly make the wounded to reengage as a combatant. If needed help the wounded to preform self-aid and move him to a relatively more secure area. If the wounded suffers from a life-threatening external haemorrhage, use a tourniquet; high and tight. Airway management is for later. Let us go through the aspects slowly step by step. According to TCCC in CUF the first priority is to stop massive haemorrhage in the wounded.

M – MASSIVE HAEMORRHAGE (OR SEVERE BLEEDING)
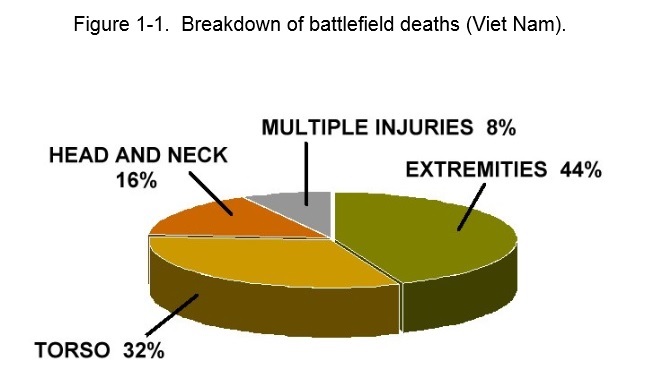
Most soldiers or persons in conflicts die due to severe bleeding. The severe bleeding comes from damage to an artery. It might be a gun wound or a cut from a knife, but more frequently it is particles or debris from different types of explosions. Materials fly through the air and cut the skin, blood vessels or amputate limbs. If a cut create a squirting red bleeding it is considered a massive haemorrhage. All massive haemorrhages normally kill before 5 minutes; meaning it is no time to lose. TCCC have only two treatments for massive haemorrhage. This is tourniquets for massive haemorrhage from extremities, and wound packing for massive haemorrhage from torso. Let us take a closer look at these two methods of handling a Massive haemorrhage.

Tourniquet
This is THE tool for treating massive haemorrhage on the extremities; arms and legs, AND only THERE. We aren’t speaking about a small bleeding from a scratch. We are speaking about major bleedings where the person is losing a lot of blood rapidly. This is a situation where a small bandage changes nothing. The person is lying in a pool of blood and death is getting closer every second. A simple tourniquet will within seconds stop any bleeding from the extremities. This tourniquet is easy to put and to manage in stressful situations. The essential function to a tourniquet is to close all blood vessels to avoid further blood loss. One of the important keys here is the risk of going into shock when you lose so much blood so quickly. An early application of a tourniquet will delay the entering into hypovolemic shock. Patients that haven’t entered shock have higher survival rates. In old times we used rope and a stick to create a tourniquet. This homemade tourniquet worked only a little on its best. The modern tactical tourniquet is a completely new world in first aid. It stops the bleeding and then the paramedic just need to transport the wounded to hospital. Another problem with tourniquet is the excessive pain it creates when it is put hard. The two less painful and most trustable systems is the windlass and the pneumatic system. Pneumatic versions of tourniquets creates less muscular and nerve damage due to less cuff pressure gradient. The benefits outweigh the risks of using tourniquet. There are three basic rules for use of tourniquet: Pressure only until total stop of blood flow, try to not use it for longer than 2 hours (it is not that dangerous to use), and finally, select a good place “high and tight proximal to the haemorrhage.

According to TCCC standard protocol the use of tourniquet is almost at an instant. Civilian EMS tells us that the use of tourniquet might cause limb amputation and nerve loss. The hard fact is that this is not true! Only 0.4% will amputate (not due to the tourniquet) and 1.5% gets nerve damage. It is no problem using a tourniquet; normally a necrosis does not come before the 2 hours limit, and some might last between 5 to 8 hours without resulting in amputation. In other words, leave the tourniquet on and search final medical treatment fast. It exist many different types of tourniquets, but the most common one are “Combat Action Tourniquet (CAT). CAT might be put single handed on you; improvised tourniquets do not work as well as the professional one, but in the need we have to improvise.
A research conducted by Eastridge, Mabry, Seguin & et al (2012) on 4,596 war fatalities between 2001 and 2011 showed that 87.3% of all injury mortality occurred pre-Military Treatment Facility (MTF). The researchers found that 3,040 of the 4,596 were classified as non-survivable, and 976 (24.3%) were potentially survivable. 90.9% of the dead suffered haemorrhage (888 persons). The site of haemorrhage was truncal (67.3%), junctional (19.2%), and peripheral-extremity (13.5%) haemorrhage. Tourniquet can be used on peripheral-extremity haemorrhage and on most junctional as well. Junctional need pressure bandage in addition, and require more training. Truncal haemorrhage is normally tactically treated with pressure bandage and Celox in the field. The most easy and preventative death is peripheral-extremity haemorrhage. As we know today tourniquets are a part of the tactical uniform (military, police, paramedical and civilian) to handle this type of injuries. Improvised tourniquets do not work as well as the tactical one; meaning we need a proper tourniquet to save life.

Wound packing
Wound packing is another way of treating haemorrhage. Tourniquets are more for extremities and wound packing is for the trunk and junctional, but you might use it with great success any place on the body. This technique involves the use of pressure on a wound directly. Normally you try to find a place where you might apply pressure against a bone. When the leak is closed the person stop bleeding. Often we find deep wounds and for that we need Celox gauze. You simply fill the hole wound with Celox (a haemostatic agent I recommend, others might recommend Quickclot/ Combat gauze) and then you put the pressure wound packing on top. Blood will flow and soak the Celox, and when it is soaked it will promote the blood coagulation. After a short time the bleeding will stop, and the wounded might be moved to a final treatment facility.

Procedure for massive haemorrhage
Requirement: A lot of blood!
- Massive haemorrhage on peripheral-extremity: Tourniquet directly
- Massive haemorrhage from trunk: Fill the hole with Celox gauze and put a pressure bandage/ wound packing on top.
- Massive haemorrhage junctional: Tourniquet on extremity and celox gauze in the wound with a wound packing/ pressure bandage on top

Don’t do more than needed in CUF wait until you reach safe territories Tactical Field Care (TFC). Then you continue with A for Airways. I must just add that sometimes you might do a little more than intended in the different levels, but try to stick to procedure. Time is an important issue and the clock is ticking… MOVE to TFC as fast as possible. Treat major bleeders first (CUF) under partial cover, then move the wounded to complete cover. First when in complete cover you might begin Tactical Field Care (the rest of MARCH); not before.

Tactical Field Care
The Second point is: Tactical Field Care (TFC). This is close to the fire, but out of the line of fire. Still hot episodes might occur, but this area is safer. When entering the area of TFC consider “SSS” – Security, Scene and Situation again. At once you enter TFC you continue with standard MARCH procedure. Most likely you are finish with M – Massive haemorrhage.

According to the standard TCCC protocol in TFC, all with an altered mental status should be disarmed immediately. Then you are supposed to take care of the airways of the wounded. Beside the normal lineation of the neck and opening of the mouth it is normal protocol to put a nasopharyngeal tube in all unconscious patients and to put them in a recovery position; accommodate if wound creates difficulties. If the airways are totally closed preform a cricothyroidotomy (Use lidocaine if conscious). With tension pneumothoraxes decompress the chest 14 G catheter. If you have oxygen tank use supplemental oxygen with 90% saturation; remember a tank is dangerous. Sometimes the patient might still bleed from an unrecognized place. Identify the origin and use tourniquet or haemostatic agent like Celox – or Combat gauze. After losing a lot of blood the wounded might need intravenous (IV); use an 18G needle. Intraosseous is an alternative to IV. When the patient is not in shock you might ship IV and give liquid to drink. The key to resuscitation is a palpable radial pulse or a systolic blood pressure of 80-90 mmHg. Sometimes an improved mental status might indicate improval of the patient. Revise the patient after every 500mL IV bolus. Beside IV it is equally important to prevent hypothermia. Put on dry clothes and lay down the patient on an isolated surface, and use a blanket; the best is a heat-reflective blanket/ shell. Often we find a pulse oximeter as a good way to monitor the patient. Then you attend minor damages and inspect everything needed. Often we find the wounded in pain. Use Tylenol 650 mg and Meloxicam 15 mg with mild pain, and if awake transmucosal Fentanyl citrate (OTFC) 800 ug. If he is in problem use Ketamine 50 mg IM or Ketamine 20 mg on slow IV. Do not stop revising the patient. Often we find soldiers to get burned. Cover the burn area with dry, sterile dressings. For extensive burns (>20%) use a Survival Blanket to prevent Hypothermia. Start with IV and fluid resuscitation; S. saline. Normally we give the % of burned x 10cc/hr. for normal adults; for every 10 kg over 80 kg add 100 ml/ hr. Sometimes the person get problem with the heart or the respiration and need Cardiopulmonary resuscitation (CPR). TCCC have a rule to be followed: Victims of blast or penetrating trauma with no pulse, no ventilations, and no other signs of life should be left for dead. Casualties with torso trauma or polytrauma who have no pulse or respirations should have bilateral needle decompression to ensure they do not have a tension pneumothorax prior to discontinuation of care. Let us go into details.
A – AIRWAY
A blocked or restricted airway might be controlled, but are the second most frequent killer due to the limited time. With no oxygen you will die within 4 minutes; making it essential in all tactical situations to unblock the airways quickly, but always after first treating a massive haemorrhage. The main key to understand airways in a tactical situation is practical and direct. Remember it is no time for fooling around and loosing valuable time on details. If the patient has some kind of sound he has clear airways. End of that problem. It is possible that he doesn’t have 100% open airways, but if they are partially open he will survive. Another problem is the unconscious patients. One of the main occurring airway problems in them are swallowing of the tongue; a totally relaxed tongue caused by unconsciousness might fold backward in the mouth and block the oesophagus. In a tactical situation we don’t have too much time to evaluate a patient. This gives us the need for procedures; to know what to do in a difficult moment.

Nasopharyngeal
The most efficient method is to use s nasopharyngeal (NAP). A NAP is easy to put and function very well. A NAP is a flexible rubber hose that you put through the nose of the patient to his throat. The technique to put it is very simple: Put the hose into one of the nostrils, and push it straight back (direction to the spine); not up. When it is all in, it is in its place. TCCC: Put NAP on all unconscious patients in TFC!
Procedure for blocked airways
Criteria: Cannot produce any sound
- Conscious wounded:
- Move the tongue (carefully).
- Heimlich manoeuvre.
- Put NAP.
- If the wounded go unconscious, continue to the unconscious wounded section
- Move to Tactical Evacuation Care (TACEVAC).

- Unconscious wounded:
- Put a NAP
- Then recuperation position
- Move to TACEVAC
- Field Tracheostomy (ONLY IF TIME AND PLACE)
- Find the Adam’s apple
- Move your finger down until you feel another bulge; 1-2 cm. This is the cricoid cartilage.
- Get a knife
- Cut 1.5 cm horizontal and 1 cm deep.
- Make the hole open with your fingers
- If trachea still not is open make a hole!
- Put a NAP into the trachea
- The tubes depth inside is about 1.5 cm.
- If needed two quick breathe into the tube every five seconds
- Move to TACEVAC
- Nada sirve
- Inicia RCP
- 100 compresiones per minuto sin parar
- Move to TACEVAC
R – RESPIRATION
We will find this point fusion with the A – airway. Loosen the clothes and observe chest movement, listen for sounds and palpate for torso movement. The main theme here is no respiration and pneumothorax.
Pneumothorax
Since most damages in tactical operations involve a type of penetration damage to the chest cavity we have the chance for damage to the pleural space. Damage might cause a collapsed lung called pneumothorax. We got two different main aspects with a pneumothorax we need pay attention to: air pressure and a penetrated thorax.

Pneumothorax: Progressive respiratory distress (Air pressure inside thorax). The air pressure builds up inside space where the lung collapsed. The first symptoms we observe are the beginning of shortness of breath and difficulties with breathing. This might be air accumulating inside the empty space after the collapsed lung; air enters but have no place to go out. We will see a progressive severe worsening in the respiration and the wounded gradually feel more and more terrible (!); a type of panic terrible sensation. Since the torso is filling with air, like a football inflates we observe the heart getting problems of beating properly and the other lung get problems with filling up normal. This is a critical situation that might lead to death. This condition is normally called progressive respiratory distress. The treatment is a simple needle decompression.

Since the problem is accumulated air inside thorax, we need to let the air out. The common way to resolve it is to put a needle (G14x10cm) three finger widths below the midpoint of the clavicle bone; directly into the space of the collapsed lung. You might feel strange putting a long needle directly into the lung cavity, but there is no lung there, only a lot of accumulated air. When the needle reaches the space you will hear a sound of air leaving the torso; like puncturing a football. This will give an instant relief for the wounded and his respiration will get better at once.

Regulate air pressure – Seal the torso
All wounds above the navel should be sealed. The best way to do this is to put your hand on the torso wound to manually medium seal it. Then you put a medical chest seal or whatever air tight material and cover the wound. Normally this is done through putting a piece of plastic over the wound, and collocate tape around the plastic. Some think it is good to seal completely with tape and others only ¾ to permit air to go out. I prefer to seal exit wound completely and entrance wound ¾. This is to prevent more air from entering as the wounded inhale, and to permit some air to get out on exhalation. Just to have mentioned it again; any bullet wound might have an exit wound – examine.

Procedure for Pneumothorax:
Criteria: The lung is punctured
Accumulated Air pressure
- Air is accumulating inside torso
- Put a needle G14x10cm directly into the lung to decompress
- Three fingers under the midpoint of the clavicle
- You will hear a sound; this indicates that the air is letting out and the wounded are getting better.
- Transport to TACEVAC

Regulate Air pressure
- Air is getting in and out of a hole in the torso
- Cover the hole(s) with plastic and secure with tape
- Entrance wound ¾ and exit wound complete
- Transport to TACEVAC

If the person simply has stopped breathing we need to start with artificial breathing. A tactical paramedic does not transport oxygen for the risk of explosion. That leaves him with only one solution waiting for the TECEVAC; Pulmonary resuscitation (PR) or cardiopulmonary resuscitation (CPR) if the person s heart does beat. The tactical paramedic will only if in a SAFE AREA do CPR or PR. The technique is to bend the head of the wounded back to open the airways, put his mouth over the open mouth of the wounded and breaths in for about 5-6 second. Then wait for 5-6 seconds and repeat. If the hear does not beat the tactical paramedic need to perform CPR. This is 30 heart compressions, then 2 inflations. This continues for 5 cycles. Then he will check vital signs; pulse and respiration.

Procedure for Cardio Pulmonary Resuscitation (CPR)
Criteria: No pulse (breathing or not is really not that important)
The heart does not beat
- Place your knees beside the torso of the wounded
- Imagine a line between the nipples and on the centre of sternum. Where the lines cross, put your right hand with the left on top.
- Start pressing down his chest, about 5 cm with a frequency of 100 times per minute.
- Press 30 times and then you give 2 inflations, 5-6 seconds each.
- Repeat 5 cycles
- Check for pulse and respiration
- If pulse and respiration – stop
- If not continue
- Transport to TACEVAC as soon as possible

C – CIRCULATION
In TCCC we treat problems with bigger bleedings under M and smaller bleedings like cuts here. The main indication of this C for circulation is the prevention of shock. To prevent shock we need to know what shock is. Normally we say that shock is a lack of perfusion of blood in our tissue. Something has created a situation that makes our tissue to receive less blood than normal. The body will do its best to adjust for the new situation, but after about one hour it will normally fail. In severe situations we only got minutes. Shock is often the precursor for death! The classical way of administrating the C in MARCHE is as BIFIT. BIFIT indicates Bleeding control, Intravenous/ intraosseous access, fluid resuscitation (HSD: volume expander) and Tourniquet assessment and removal.
One of the easiest indicators for shock is to take the radial pulse. If a pulse we know that the body still pump blood to the extremities and if no pulse we know that the body have problems with maintaining the blood flow in the body and is likely to go into shock shortly. Preventative treatment is needed. Normal preventive actions are to stop massive haemorrhage, regulate the airways and respiration, intravenous therapy (IV) and heat. A tactical paramedic will only start with IV if he considers it safe.

IV has got a lot of attention recently. The new standard is to give whole blood products (WBP) while others prefer to fill the patient with an almost unlimited amount of bags of crystalline. The trend today is to reduce the amount of crystalline to avoid bleeding and to maintain a mean arterial pressure (MAP) of 50 mmHg; exactly high enough to maintain the blood flow to the vital organs and exactly low enough to limit the excessive bleeding. The origin to this trend is founded in the ideas of damage control resuscitation (DCR). The key points are to maintain an average of 80 mmHg in systolic pressure, use frozen fresh plasma (FFP) IV as early as possible, and about 150ccc crystalloid IV. Monitor and control MAP will control the bleeding; ((2 x diastolic) + systolic) / 3. A better controlled MAP will increase the chance for survival. Still we do not know the optimal blood pressure when a person bleed, but we know that a too high pressure creates an increased bleeding and too little blood damage the organs. The Tactical paramedic observes the patient on three aspects: a non-palpable radial pulse, an altered consciousness and change of blood pressure. The key is to stop IV when the radial pulse becomes palpable. Normally this is after 150 mL normal saline (0.9% NaCl). Some put the maximum limit of normal saline to 20 mL/ kg (EG. 100 kg body weight = 2000 mL or 60 kg = 1200 mL). If the patient stops bleeding, you stop IV with the arrival of the radial pulse. If the patient continues bleeding, continue with a moderate IV.

H – HEAD/ HYPOTHERMIA
HEAD
The head is often injured on the battlefield. The head is not that frequent hit by a bullet, but more frequent a victim of explosions. When injured in the head the essence is covered through the other letters M-A-R-C, but this H give the head some more attention.

The classical Traumatic Brain Injury (TBI) might be everything from an altered mental state, different size on the pupils, yellow liquid leaking from the orifices of the head, deformations on the head, and “raccoon eye” (bruises around the eyes). Since not all damages to the head is that visible the tactical paramedic will have to review carefully. This damage is not for treating in the field. If TBI is discovered inform in TECEVAC.
Hypothermia
All persons wounded will get cold when they lose blood; the loss of blood will also reduce the ability of the body to produce body heat. Hypothermia might occur in any climate; not only cold climates. That is why you need to dress the wounded after examined the body. If possible add additional clothing or a blanket. Keep the wounded warm!
When you are finish with administrating MARCH, then you do E – everything else; this mean to prevent other or further damages. This might be everything from calming down the wounded or putting more bandages. Of course, if needed engaging in combat again.
Eviscerations
Sometimes in combat we might experience wounds where organs are hang out; this is called evisceration. Normally it is the intestines that hang out. This is not directly dangerous since this is not a massive haemorrhage but rather an organ that is located different than normal. Of course, with time we might get infections and other complications and organs should not be located like this. TCCC have strict protocols for eviscerations. We are supposed to put them back inside the womb again; before we should keep them outside. Before we put them in we should clean them with a clean solution. And after putting the viscera in we need to close the wound with bandages to prevent them to fall out again. When reaching final hospital they will clean the womb of the patient and disinfect. It is overall safer to have the viscera’s inside than outside in a plastic bag running in the forest.

Tactical Evacuation Care (TACEVAC)
Some place here we reach TACEVAC, and we start moving away from the hot area. Perhaps we still are putting an IV or we are doing something else. Everything depends. Tactical operations are unpredictable by nature and might take some minutes or days. This indicates TACEVAC might come in an instant or in two days. If it lasts hours and days the tactical paramedic has to start working with more medical procedures than what is constituted by a classical paramedic and standard EMS. Let us look at some of these topics.

According to TCCC directive at TACEVAC we will have both a casualty evaluation (CASEVAC) and a medical evaluation (MEDEVAC). It is a classical ABC evaluation with the standard intervention. When hypovolemic shock and you need IV you give whole blood or crystalloid (Hextend, Lactated Ringers or Plasma-Lyte A). If the person is awake you better give oral liquid, and if the person is not in shock you don’t need IV. If you give IV you need to revise the patient after every unit (500mL) for radial pulse, improved mental status and a minimum 80-90 mmHg in systolic blood pressure. Stop IV if one of the above is okay. It is important to prevent hypothermia. Monitor the patient with a pulse oximeter. While waiting you inspect, dress and check for additional wounds. If indicated and needed give medicaments. If the patient got problems with the respiration, revise for a tension pneumothorax; decompress with a 14G needle. If the person needs CPR do CPR, but only if the patient do not have fatal wounds and will arrive at hospital very soon.
E – EYE INJURY AND EVERYTHING ELSE
Here we find a huge amount of what ever to treat before reaching the hospital. Very important here is the word M-PHAAT-D that sum up everything else. M-PHAAT-D indicates Monitoring, Pain, Head to toe, Address all wounds, Antibiotics, Tactical evacuation preparation and Documentation of care. This does indicate that the tactical paramedic will continue working for the wounded until he is safe in hospital.
Smaller haemorrhages
This is a wound that does not create a life threatening situation. An example of these wounds might be a cut to the head and basically everything that is not on the inside of the body; forearm, legs, buttock, shoulders and lateral spine. Remember that arteries are located on the inside of our extremities and often close to bones and muscles. The location often provides some protection against haemorrhage. Is a minor haemorrhage we normally treat it sufficiently well with a normal bandage.
Saw a wound
If TACEVAC lasts we need to consider sawing together a deep wound. Everything depends on how deep it is and the risk for infection. To saw a wound fills two purposes: First of all it heals better (tactically irrelevant) and secondly it reduces the risk of infection and it help against bleeding. The risk of infection is one of the main indicators for us. If the wound have been contaminated by dirt, pus, bites or whatever, or is longer than 5 cm we need to clean it deeply. If we find a wound becoming swelled, red and painful we have a sign of infection. Often we find a formation of pus, an uncomfortable sensation, swollen glands and fever. In the civilian life we have the 1 mm rule; 1 mm deep or 1mm wide, and the 1 hour rule; bleeds for more than one hour. Try first to disinfect the wound and bandage. If you know it will take more than 24 hours for the wounded to get to hospital and the wound need to undergo a minor surgery; you might consider doing some field sawing of a wound. The cut need to be deep and long, and within your abilities. This is just for special situations; remember that!!!

Procedure for Field Sawing a wound
Criteria: No other option
Long deep open cut
- Disinfect your hands
- Clean the wound
- Disinfect the cut
- Small wounds; close with sticker or strip called “Butterfly”
- Bigger wounds; close with stitches
- Make your equipment ready
- Inject Lidocaína 10 mg/ ml with an insulin needle
- Use Continous stitch; make nice stitches and make sure the parts closes well.
- Put a steril bandage on top
- Antibiotica is recomendable for one week
- In one week you take away the stitches